Oophorectomy
What is an oophorectomy?
 Oophorectomy Definition
Oophorectomy Definition
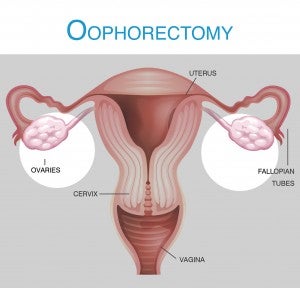
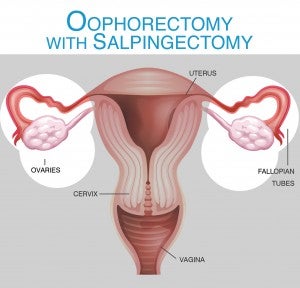
An oophorectomy is the surgical removal of an ovary. When one ovary is removed, it is referred to as a unilateral oophorectomy; when both are removed, it is called a bilateral oophorectomy. A salpingectomy (removal of the fallopian tubes) and/or hysterectomy can be performed along with an oophorectomy, or the surgery can be done separately.
Surgical Choices of Oophorectomy
Similar to a hysterectomy, an oophorectomy is done using several different methods in a surgical center under anesthesia. A laparotomy is the most invasive option and involves a single, larger incision in the lower abdomen. For this type of oophorectomy, the hospital stay and recovery will be longer. There will be extended post-operative pain and the scar will be more significant. Recovery and restrictions may last as long as 6 weeks, similar to an abdominal hysterectomy.
Minimally invasive options, such as a laparoscopy, may use a single belly button incision or a few small incisions in the abdomen area, which can minimize scarring, decrease pain, and shorten recovery. This type of surgery may also be performed on an outpatient basis so that no overnight hospital stay is required. Recovery can be between 2–4 weeks.
An oophorectomy may be done for benign conditions, malignancy, or prophylactically when there is a specific higher risk of cancer. As new research is indicating that ovarian cancer may begin in the fallopian tubes, some women and their medical professionals may decide a prophylactic salpingectomy rather than a prophylactic oophorectomy is the right choice. More research is needed, however, to determine if this should be a universal recommendation.
 Oophorectomy Risks
Oophorectomy Risks
General risks for an oophorectomy include infection, bleeding, nicking nearby organs, and small bowel obstruction. In addition, if ovarian cells are missed ovarian remnant syndrome (ORS) can occur, which can lead to continue ovarian issues and even ovarian cysts. As with any surgery, there can also be anesthesia or medication reactions.
Outcome: Removal of Both Ovaries Creates Surgical Menopause
The ovaries produce estrogen and progesterone. Removal of both ovaries causes surgical menopause. Health risks involved losing those hormones include vaginal dryness, heart disease, osteoporosis, and premature death. Depression, mental issues, and decreased libido may also occur, along with hot flashes, night sweats, and fatigue. In some cases hormone replacement therapy (HRT) may be an option and could minimize symptoms, but HRT is not right for everyone and comes with some pros and cons, too.
If your ovaries are healthy and you do not have a family history of ovarian cancer or breast cancer, keeping your ovaries is advised.
If an oophorectomy has been recommended for you, consider seeking a second opinion before scheduling surgery to help you determine if this surgery is right for you. You’ll also want to weigh all the pros and cons and consider the long-term hormonal implications before making any final decisions.