There are 3 important decisions related to a hysterectomy:
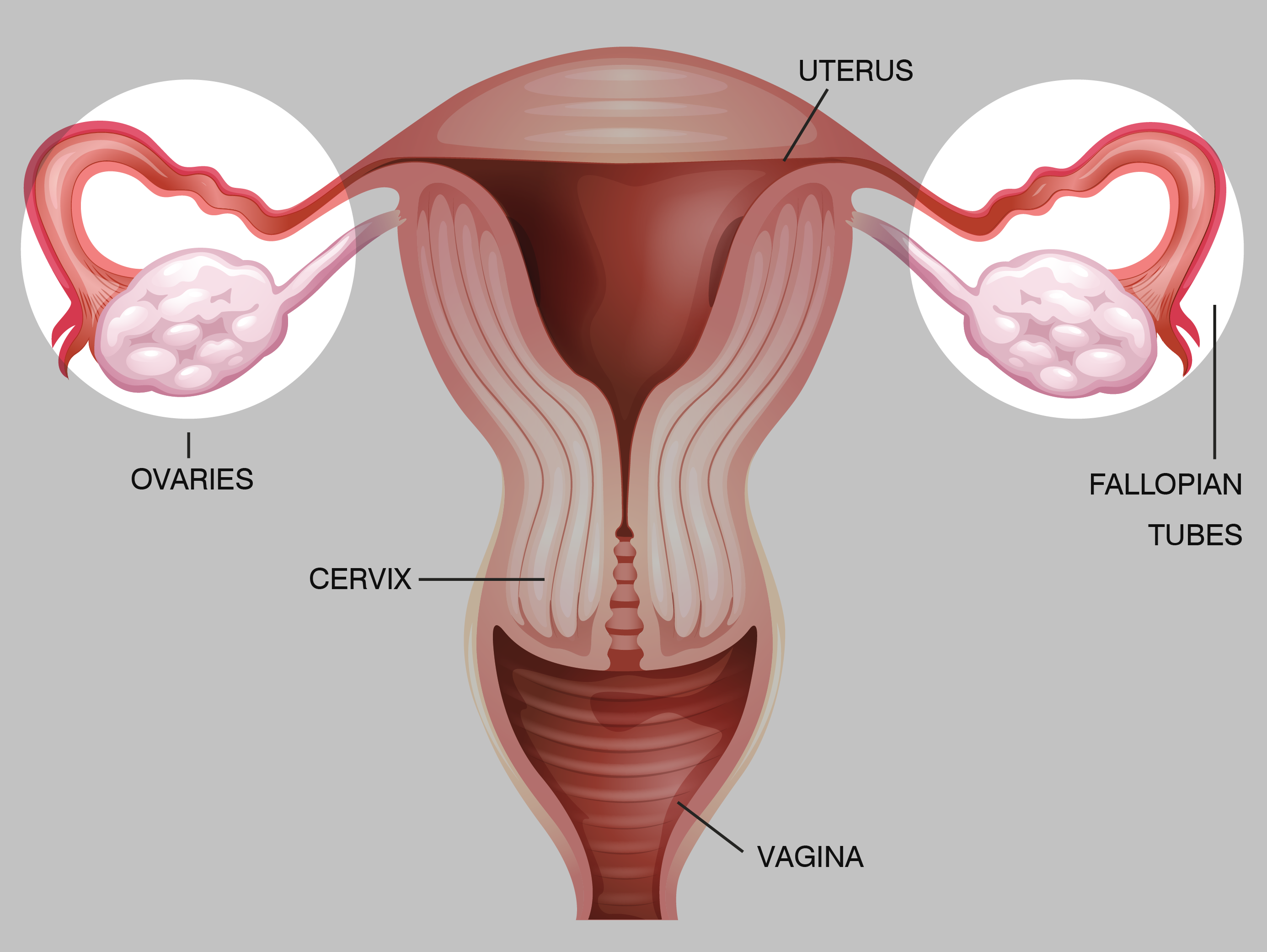
1. Should I keep my cervix?
2. Should I keep my ovaries/tubes?
3. What type of hysterectomy should I have?
the surgical removal of the uterus, otherwise known as the womb. Thankfully, a hysterectomy is rarely an emergency surgery, so women usually have time to learn about their options and choices before going into the operating room. The more you know about your choices, the better decisions you can make for your immediate and long term health. Always consult a surgeon who specializes in GYN surgery. The three choices you’ll need to make concern your cervix, ovaries, and the type of hysterectomy.
The first decision you need to make is whether or not you will be keeping your cervix when you have your hysterectomy. The cervix is the bottom part of the uterus so it can be removed along with the rest of the uterus or be cut from the fundus (upper portion) and retained.
Diseased or Healthy?
Your specific diagnosis may play a role in whether or not you will have the option to keep your cervix; the issue affecting the fundus may also be affecting the cervix. Diagnoses such as HPV, abnormal uterine bleeding, or cancer are examples of diagnoses which may require the removal of the cervix along with the rest of the uterus. Many doctors also recommend the removal of the cervix for endometriosis or adenomyosis diagnoses.
If your cervix is considered unaffected by your diagnosis, then you will need to determine if the pros outweigh the cons for retaining it. There are mixed opinions from both women and medical professionals regarding whether or not there are benefits to keeping the cervix after a hysterectomy, so it is very important that you speak to your doctor and get a second opinion about what is right for you. This can be a very personal decision, so feel free to talk to your doctor about your thoughts, concerns, and feelings so you can make the best decision for you.
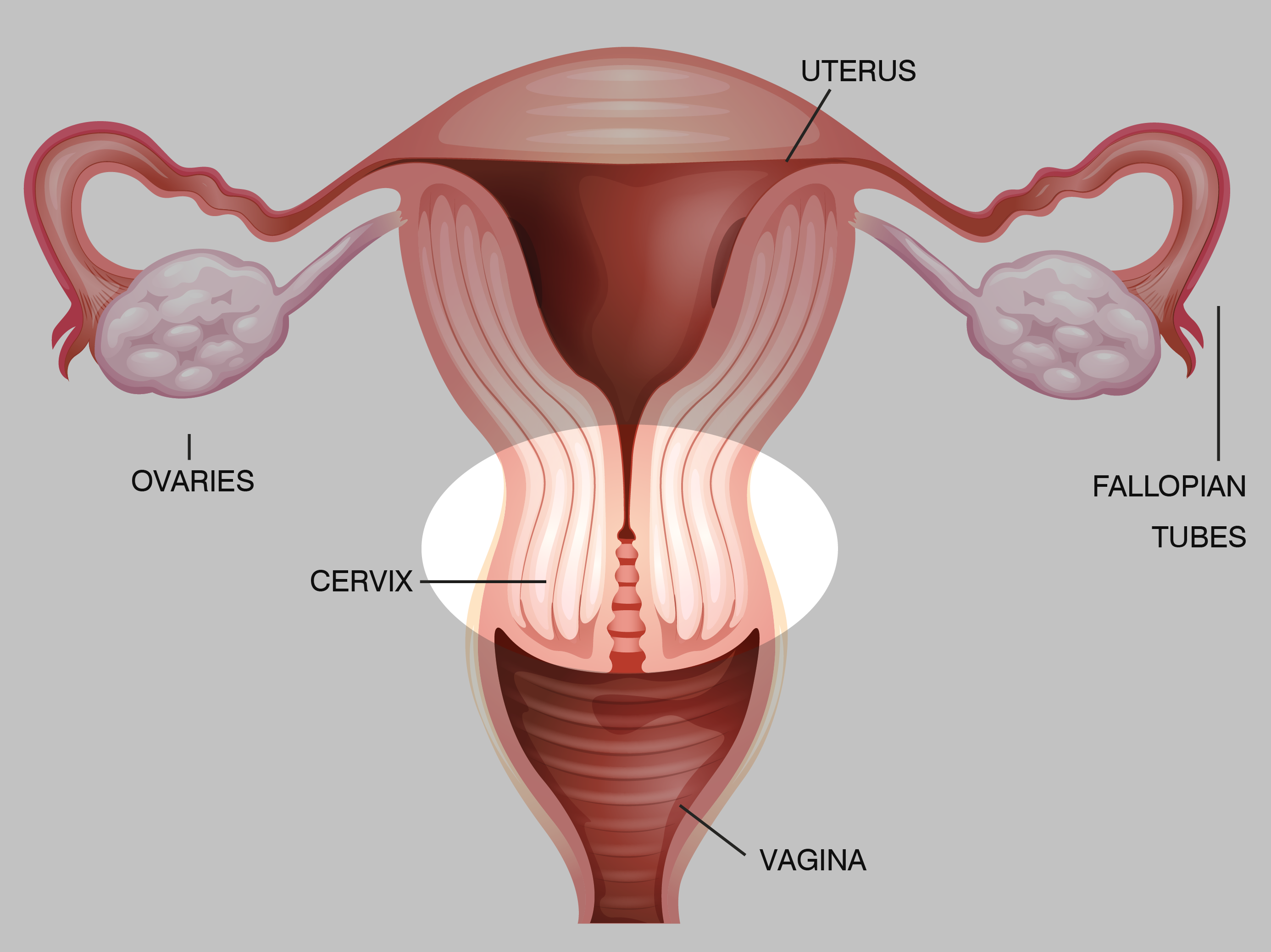
Another choice you’ll need to make is whether or not to keep your ovaries. The younger you are, the more critical it can be to keep your healthy ovaries as estrogen plays a critical role in overall health.
Age, Overall Health, Genetics
Besides age, there are several other factors you’ll need to consider when making this decision. Are you a candidate for hormone replacement therapy (HRT)? Do you have underlying health issues which will be impacted by an oophorectomy? If you have certain diagnoses, genetic issues, or cancer concerns, then your pros and cons will be affected by those conditions. It can be helpful to consult with a medical professional who specializes in your condition so together you can determine how an oophorectomy might help or worsen your situation. In addition, research has indicated health risks related to oophorectomies for benign reasons. These health issues can include heart concerns, osteoporosis, mental issues, premature death, and more. Using HRT can help minimize some of the risks, but you’ll need to consider those concerns before making your final decision.If you are close to or in menopause, you may feel the ovaries are no longer necessary. However, the ovaries can still secrete trace hormones during those menopausal days. If your ovaries are healthy, the pros of removing them may not outweigh the cons of the new health issues you may face.
Salpingectomy – Tubes Removed:
Whether or not you decide to keep or remove your ovaries, you can also discuss a salpingectomy (removal of the fallopian tubes) with your doctor. If your fallopian tubes are blocked or diseased, your doctor may recommend having the fallopian tubes removed. In addition, studies have found that ovarian cancer in the fallopian tubes. As a result, some doctors automatically recommend the fallopian tubes be removed during a hysterectomy, while others are recommending it for those with a personal or family history of ovarian cancer.Before making a final decision about your ovaries and tubes, it can be helpful to get a second opinion. It can also be helpful to speak to your general practitioner about your overall health and any conditions you have which are affected by your hormones. Removal of the ovaries can impact your health from head-to-toe, so you’ll want to do your best to make the right decision for you.
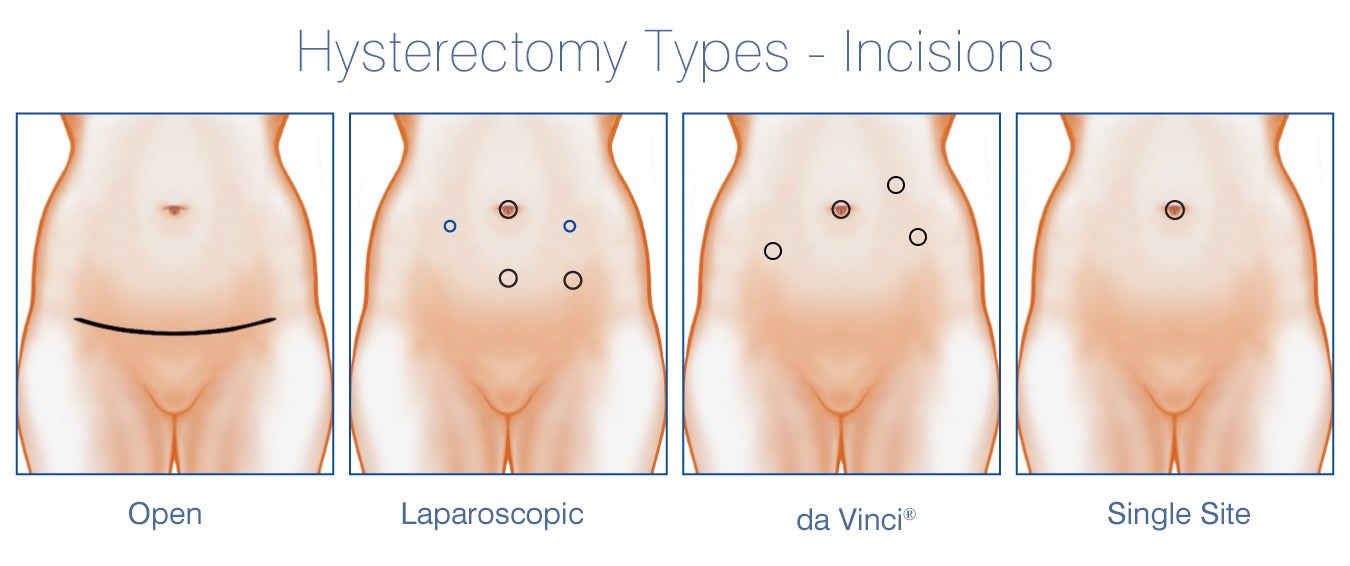
Surgery Types for Hysterectomy Include:
da Vinci®
da Vinci® hysterectomy is a minimally invasive surgery using a robotic tool which increases visibility while minimizing incision size. Recovery time is typically 2-4 weeks.
Laparoscopic Assisted Vaginal
Laparoscopic Assisted Vaginal hysterectomy is a minimally invasive surgery which combines vaginal and laparoscopic techniques to remove the uterus. Recovery time is typically 2-4 weeks.
Laparoscopic Supracervical
Laparoscopic Supracervical hysterectomy is a minimally invasive surgery using laparoscopic techniques to remove the top portion of the uterus while preserving the cervix. Recovery time is typically 2-4 weeks.
Total Laparoscopic
Total Laparoscopic hysterectomy is a minimally invasive surgery, removing the total uterus using laparoscopic techniques and small incisions. Recovery time is typically 3 – 5 weeks.
Single Site Incision
Single Site Incision hysterectomy is a minimally invasive laparoscopic surgery completed through a single incision in the belly button. Recovery is typically 3-5 weeks.
Supracervical Abdominal
Supracervical Abdominal hysterectomy is the removal of the upper portion of the uterus through an open abdominal incision. Because abdominal surgery is not minimally invasive, recovery is typically 6-8 weeks.
Total Abdominal
Total Abdominal hysterectomy is the removal of the entire uterus through an open abdominal incision. Because abdominal surgery is not minimally invasive, recovery is typically 6-8 weeks.
Vaginal
Vaginal hysterectomy is a minimally invasive surgery done completely through the vagina. Recovery is typically 2-5 weeks.